
Are you experiencing pelvic pain and looking for expert care? You’re in the right place to understand the causes, symptoms, diagnosis, and treatment options for pelvic pain.
This comprehensive overview addresses everything from gynecological issues to musculoskeletal causes that lead to pelvic pain. Discover how our specialist, Andre Tulip, effectively manages this condition.
Learn what to expect during pelvic pain therapy sessions and how you can book your appointment. We also address common concerns about when to seek medical assistance and the impact of stress and anxiety on pelvic discomfort.
What is Pelvic Pain?
Pelvic pain affects the lower abdomen and pelvic region, potentially involving the womb, bladder, and ovaries. It can be acute or chronic and significantly impacts health and quality of life. Understanding its multifaceted nature is essential for identifying its causes and seeking appropriate treatment.
What Causes Pelvic Pain?
Pelvic pain stems from various sources, including gynaecological issues, urinary tract infections, digestive problems, musculoskeletal disorders, and psychological factors.
Gynecological Conditions
Conditions such as endometriosis and fibroids are significant contributors to pelvic pain. Endometriosis, where tissue akin to the uterine lining grows externally, and fibroids, non-cancerous growths in the uterus, cause symptoms like pelvic pressure and abnormal bleeding. Early recognition of these symptoms is key for effective treatment.
Urinary Tract Infections
Urinary tract infections (UTIs) also lead to severe pelvic pain, mainly impacting the bladder. Symptoms such as frequent urination and pain arise from bacterial infections. Treating these with antibiotics is crucial for managing the pain and ensuring accurate diagnosis.
Digestive Issues
Conditions like irritable bowel syndrome (IBS), Crohn’s disease, and ulcerative colitis also lead to chronic pelvic pain, presenting symptoms like bloating and abdominal discomfort. These necessitate thorough medical evaluations to develop appropriate treatment strategies.
Musculoskeletal Issues
Pelvic floor muscle dysfunctions contribute to pelvic pain, benefiting from targeted physiotherapy. Effective physiotherapy addresses muscle imbalances or dysfunctions, significantly easing symptoms and enhancing quality of life.
Psychological Factors
Stress and depression can intensify pelvic pain, underscoring the importance of psychological support in treatment. Managing these psychological aspects can reduce pain intensity and improve overall well-being.
Each cause affects the body differently, necessitating targeted diagnosis to identify symptoms accurately.
What are the Symptoms of Pelvic Pain?
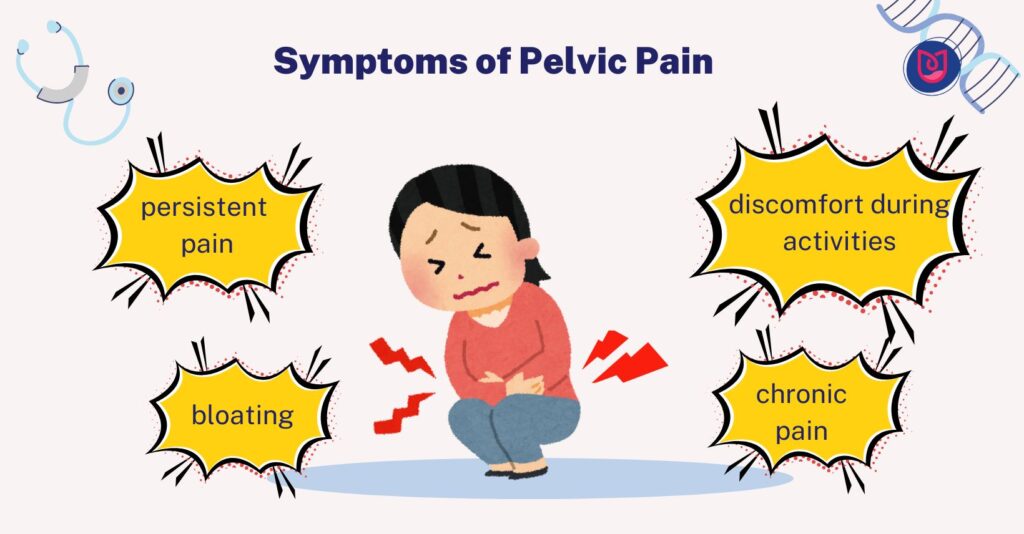
Pelvic pain symptoms vary but commonly include persistent pain, discomfort during activities, and chronic pain impacting daily life. Symptoms like bloating and urinary urgency further complicate the condition, necessitating comprehensive diagnostic approaches to identify the root causes effectively.
How is Pelvic Pain Diagnosed?
Diagnosis involves tests such as blood and urine analysis, physical examinations, and imaging like ultrasound and CT scans. These techniques help identify infections, inflammations, and structural abnormalities, which are essential for crafting effective treatment plans.
How is Pelvic Pain Treated?
Treatment options include medications, surgery, physiotherapy, and lifestyle changes tailored to the identified causes. Addressing these with a multidisciplinary approach ensures comprehensive care, highlighting why expert involvement is critical for effective management.
Why Should You Seek a Physiotherapist to Treat Pelvic Pain?
Seeking physiotherapists is vital in treating pelvic pain due to the complex nature of its causes and symptoms. Specialists from various fields contribute to a well-rounded treatment approach, ensuring all aspects of the condition are addressed. This is important when considering what to expect during treatment sessions with specialists like Andre Tulip.
What to Expect During Pelvic Pain Treatment with Andre Tulip?
Treatment with Andre Tulip involves a personalised plan focusing on physiotherapy and supportive therapies. Patients receive targeted treatments to improve pelvic health, which is essential for effective pain management and long-term well-being. This prompts those affected to take the next step toward recovery by booking an appointment.
Ready for a Therapy Session with Andre Tulip? Book Your Appointment Today!
Embark on your journey to better health by scheduling an appointment with Andre Tulip. Benefit from his expertise in pelvic pain treatment through a personalised approach, ensuring each patient’s unique needs are met, and begin your path to recovery and improved quality of life at Physio Sunderland.
Frequently Asked Questions
How do you make knee pain go away?
Alleviating knee pain often entails a mix of rest, physiotherapy, proper use of painkillers, and sometimes medical or surgical interventions. Resting initially helps the joint heal, avoiding activities that exacerbate the pain. Gentle exercises such as swimming or cycling improve muscle strength and knee flexibility. Physiotherapy, important in recovery, involves a therapist devising an exercise plan to enhance mobility and reduce pain, focusing on stretching, strengthening, and balance.
Is walking beneficial for knee pain?
Walking can aid knee pain by maintaining joint mobility and strengthening surrounding muscles, provided it’s done correctly and in moderation. It improves circulation, eases joint stiffness, and helps with weight management, reducing knee stress. Proper footwear is essential for shock absorption, and stretching before and after walking prevents injuries. Proper posture and stride reduce knee strain.
Do squats help knee pain?
Proper squat technique can strengthen the knee muscles, helping alleviate pain. Proper technique is vital; ensure your knees don’t extend beyond your toes to minimise knee pressure. Keep your back straight and core engaged to improve knee stability and flexibility. Consider lower-impact exercises like leg presses, step-ups, or wall sits for severe knee pain to strengthen without strain.
What to take for knee pain?
Over-the-counter painkillers like ibuprofen or paracetamol are effective for knee pain relief. Still, they should be used responsibly and under guidance for persistent pain. These medications reduce inflammation and discomfort, but potential side effects include stomach upset and liver damage. Always consult a healthcare provider before starting any medication to ensure it’s safe and appropriate for your needs.
Can I continue my daily activities during knee pain treatment with Andre Tulip?
Andre Tulip generally encourages continuing daily activities during knee pain treatment, with modifications to avoid aggravating the knee. Following his advice ensures optimal recovery.
How long does it take to recover from knee pain treatment with Andre Tulip?
Recovery from knee pain treatment with Andre Tulip varies based on the severity of the condition and the specific treatment plan, focusing on comfort and efficient recovery.